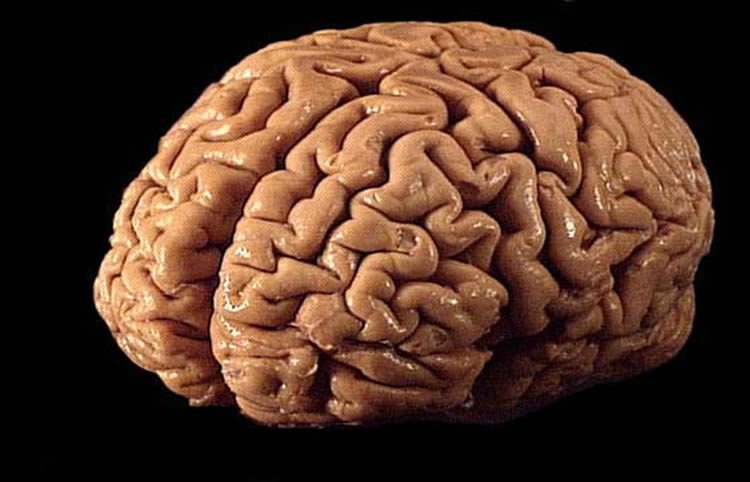
Yeast Infection May Be Linked To High Risk For Bipolar Disorder, Schizophrenia
Having a yeast infection is associated with a higher risk of developing schizophrenia and bipolar disorder, a new study has shown.
Researchers from the Johns Hopkins University have found that incidence
CorporateChrist