The Neuroscientist Who Lost Her Mind
Struck by a brain tumour, she truly grasped how terrifying life can be for the mentally ill
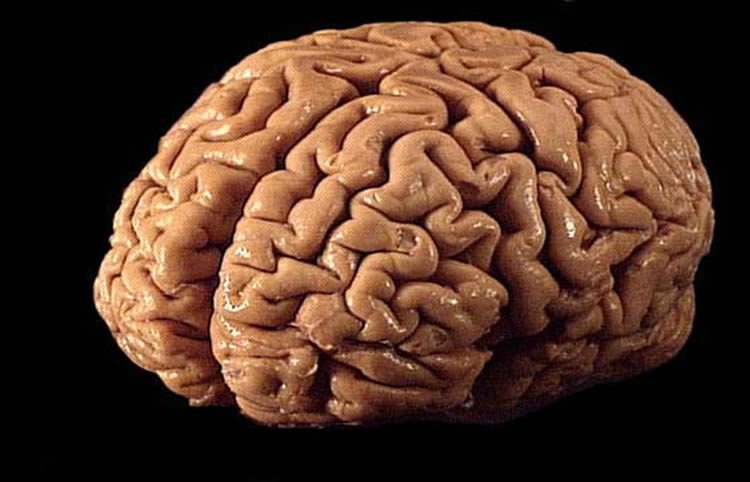
As the director of the human brain bank at the United States National Institute
CorporateChrist